How optical filters help detect stroke risk
The Stroke Association is urging everyone to Make May Purple for Stroke by wearing purple clothes, cooking purple foods, donating to stroke charities and raising awareness, as part of a month-long drive to improve early stroke detection and patient outcomes.
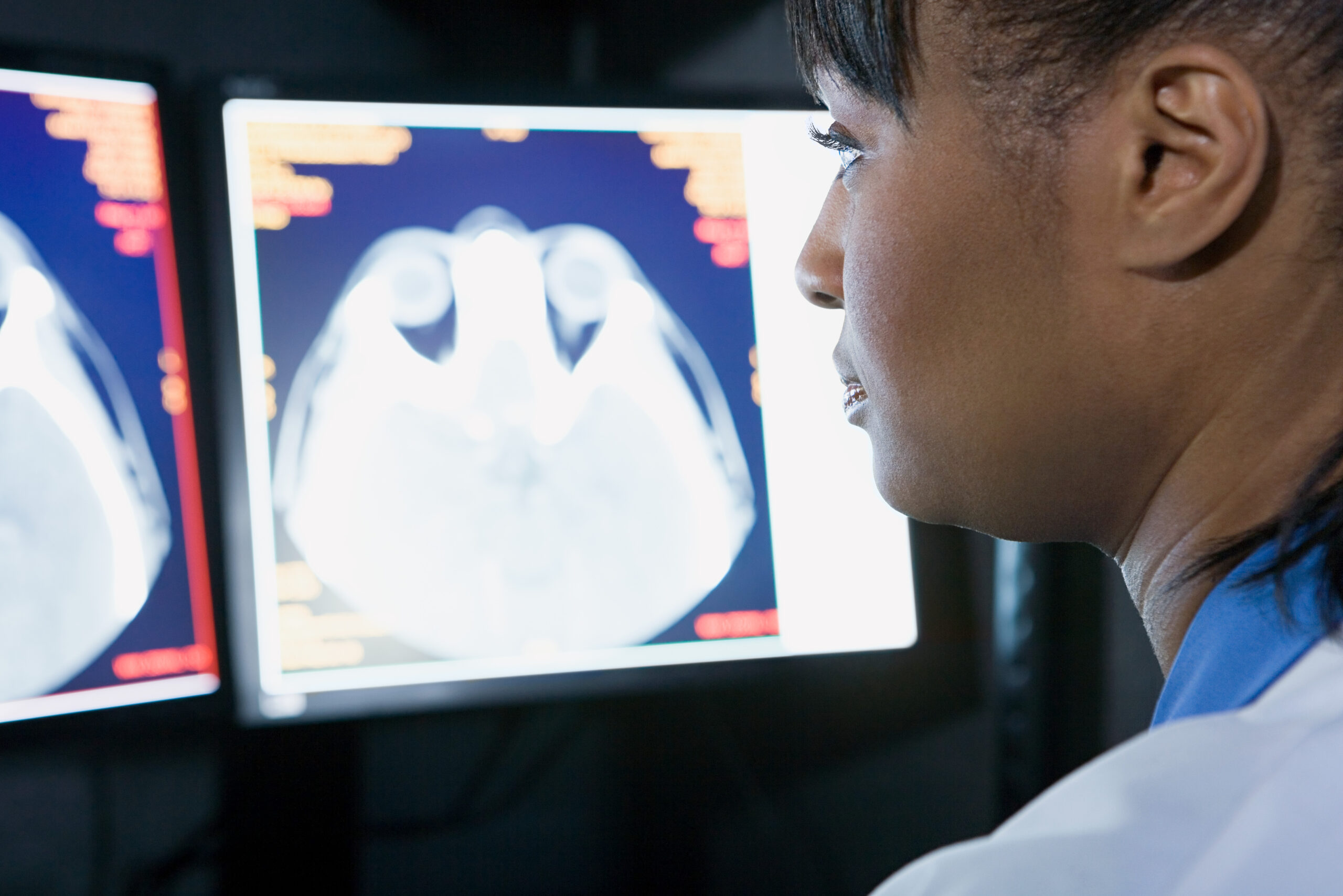
But it is the other side of the colour wheel that can be most helpful when it comes to optical filters for stroke surgery, combining near infrared imaging with indocyanine green fluorescence to picture vascular flow and help distinguish blood vessels from other tissue types.
This is beneficial during vascular neurosurgery, for example when operating to remove an aneurysm or other blockage during an occurrence of ischemic stroke, but historically the method was only able to generate a flat monochrome image of the area.
Anatomical details and real time blood flow
In recent years the limitations of this method have started to be overcome too, such as the challenge of providing full-colour imagery and of imaging both anatomical detail and real-time blood flow in a way that is more useful to neurosurgeons during the operation itself.
As a result, surgeons are increasingly able to operate on stroke patients using a single imaging technique with colour, depth and anatomical detail, and without having to interrupt a procedure to consult a 2D infrared image.
Optical filters near infrared are a key part of this, featuring in augmented reality fluorescence filters that enable the essential imaging of cerebral blood flow and anatomy for fine vascular neurosurgery to be carried out.
Implications in neurosurgery
This has broader implications for aftercare following any kind of neurosurgery, by helping to identify blood vessels in the brain that could be at higher risk of either ischemic or haemorrhagic stroke during the days after an operation.
Postneurosurgical stroke risk fell from 1.2% in 2006 to 0.5% by 2013, according to a study in World Neurosurgery in September 2016, and carefully monitoring for these kinds of risks can help to improve outcomes for all neurosurgery patients in the years to come.
Over the same period, the article noted that the percentage of patients who experience post-surgery comas over 24 hours in duration fell from 0.9% to just 0.002% – a further indication of how improved techniques and anticipation of risks are saving lives and safeguarding patients’ futures.
For more information on our range of optical filters including custom filters to help meet unique specifications, please get in touch and we will be happy to help.